Table of Contents
- Understanding the Cumulative Effects of Multiple Shocks on the Human Body
- Comparing Physiological Responses Between Single and Repeated Shock Events
- Strategies for Mitigating Long-Term Health Risks Associated with Multiple Shocks
- Guidelines for Medical Professionals in Diagnosing and Treating Shock-Induced Complications
- Concluding Remarks
Understanding the Cumulative Effects of Multiple Shocks on the Human Body
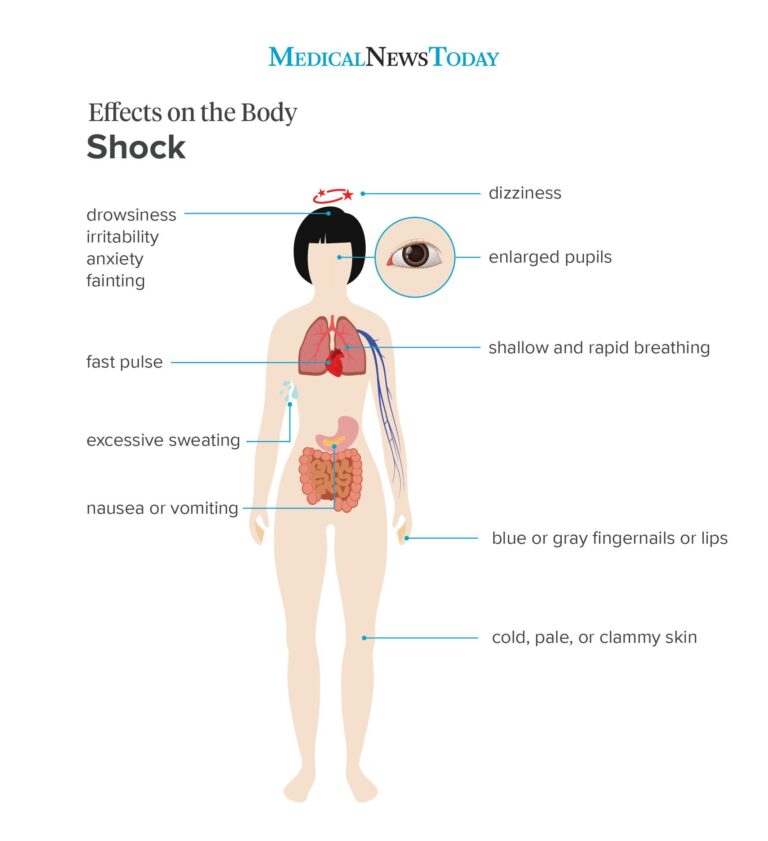
When the body experiences multiple shocks rather than a single incident, the physiological response becomes more complex and often more severe. Each shock – whether physical trauma, emotional distress, or sudden environmental change – triggers a cascade of reactions in the nervous and endocrine systems. Over time, repeated shocks can overwhelm the body’s capacity to recover, leading to a state of chronic stress or systemic imbalance. Unlike one isolated shock, cumulative shocks don’t just add up linearly but can interact in unpredictable ways, compounding the damage and weakening natural defense mechanisms. This can manifest as a heightened inflammatory response, impaired immune function, or prolonged hormonal disruption.
Understanding these layered effects is crucial for both medical professionals and individuals alike. Some key elements to consider include:
- Neurochemical Exhaustion: Repeated activation of stress pathways can deplete essential neurotransmitters and hormones, impacting mood and cognitive function.
- Tissue Vulnerability: Continuous strain makes muscles, joints, and organs more susceptible to injury and slower to heal.
- Immune Dysregulation: The immune system may become either hyperactive, leading to inflammation, or suppressed, increasing vulnerability to infections.
- Psychological Impact: The mental toll of enduring multiple shocks often amplifies anxiety and post-traumatic stress symptoms, complicating recovery further.
Comparing Physiological Responses Between Single and Repeated Shock Events
When the body experiences a single shock event, the immediate physiological response is typically abrupt and intense, characterized by a surge in the sympathetic nervous system activity. This triggers the release of stress hormones like adrenaline and cortisol, increasing heart rate, blood pressure, and respiration to prepare the body for a rapid reaction. However, this acute response tends to be short-lived, allowing the system to stabilize relatively quickly once the threat subsides. The body’s ability to return to baseline after a single shock is crucial for maintaining overall homeostasis and preventing long-term damage.
In contrast, repeated shock events produce a more complex and potentially harmful pattern of physiological changes. Instead of a single spike, the stress response becomes cyclical or sustained, leading to:
- Chronic elevation of stress hormones, which can wear down the cardiovascular system over time.
- Persistent inflammation, impairing immune function and increasing vulnerability to illness.
- Heightened nervous system sensitivity, resulting in amplified responses to even minor stimuli.
Strategies for Mitigating Long-Term Health Risks Associated with Multiple Shocks
Addressing the compounded effects of multiple physiological shocks requires a holistic approach that prioritizes resilience and physiological balance. Integrating regular stress management techniques such as mindfulness meditation, yoga, and biofeedback can recalibrate the body’s stress response systems, effectively reducing the risk of chronic inflammation and cardiovascular strain. Additionally, a tailored nutrition plan rich in antioxidants, omega-3 fatty acids, and essential vitamins supports cellular repair mechanisms and mitigates oxidative damage intensified by recurrent shocks.
Building sustainable long-term health also hinges on proactive monitoring and early intervention. Incorporating routine health assessments including cardiovascular screenings, hormonal evaluations, and immune function tests allows for the timely detection of dysregulations that multiple shocks may exacerbate. Complementing this with targeted physical activity-focusing on low-impact strength and endurance training-enhances adaptive capacity without overwhelming the system. Ultimately, fostering a supportive environment through quality sleep, social connection, and psychological counseling is equally vital, as it strengthens both mental and physical defenses against the cumulative burden of repeated shocks.
Guidelines for Medical Professionals in Diagnosing and Treating Shock-Induced Complications
When managing patients who present with shock-induced complications, it is critical to recognize that multiple episodes of shock can cause a cumulative and more complex physiological impact compared to a single event. Medical professionals should be vigilant for signs of progressive organ dysfunction, as repeated shocks often lead to exacerbated hypoperfusion and amplified inflammatory responses. This necessitates close monitoring of vital signs, continuous assessment of organ function through laboratory markers, and tailored hemodynamic support strategies that differ from standard single-shock protocols.
Effective treatment hinges on a comprehensive approach that includes:
- Early identification of secondary complications such as acute kidney injury or coagulopathy, which are more prevalent with recurrent shock episodes
- Use of targeted therapies aimed at stabilizing mitochondrial function and reducing oxidative stress
- Implementing multidisciplinary critical care interventions including advanced hemodynamic monitoring and individualized fluid resuscitation plans
- Continuous reevaluation and adjustment of vasopressor and inotropic support to prevent further tissue injury
By acknowledging these multifaceted challenges, clinicians can improve outcomes through prompt, precise, and dynamic management tailored to the unique pathophysiology induced by multiple shock events.
Concluding Remarks
In understanding how multiple shocks impact the body differently than a single event, it becomes clear that the cumulative effects can be both profound and complex. Each additional shock doesn’t just add strain-it can alter the body’s response, resilience, and recovery processes in unique ways. Recognizing these differences is crucial for healthcare providers, patients, and caregivers alike, as it informs more tailored treatment and prevention strategies. As research continues to evolve, staying informed will empower us to better support those facing the challenges of multiple traumatic experiences. Thanks for reading, and stay curious about the incredible ways our bodies navigate and adapt to stress.Check Our Other Blogs
- StunGun – Your Trusted Source for Stun Guns, Laws, and Self-Defense Tips
- PepperSprayLaws – Your Trusted Resource for Pepper Spray Information
- StunGunLaws – Your Trusted Guide to Stun Gun Legality and Safety